- Shock is a circulatory failure that happens when the organs and body tissues do not receive enough blood flow to support their oxygen and metabolic demands and purring them at risk of hypoxia and cellular injury
What are the 4 main types of shock? What are the main types of Distributive Shock?
- Distributive shock: also known as vasodilatory shock: systemic vasodilation and decreased blood flow to vital organs such as the brain, and kidneys. It also causes fluid to leak from the capillaries into the surrounding. causes tissue perfusion. life-threatening and requires immediate medical attention.
- Cardiogenic shock:failure of the heart to pump
- Hypovolemic shock: intravascular volume loss
- Obstructive shock: the physical obstruction of blood circulation and inadequate blood oxygenation
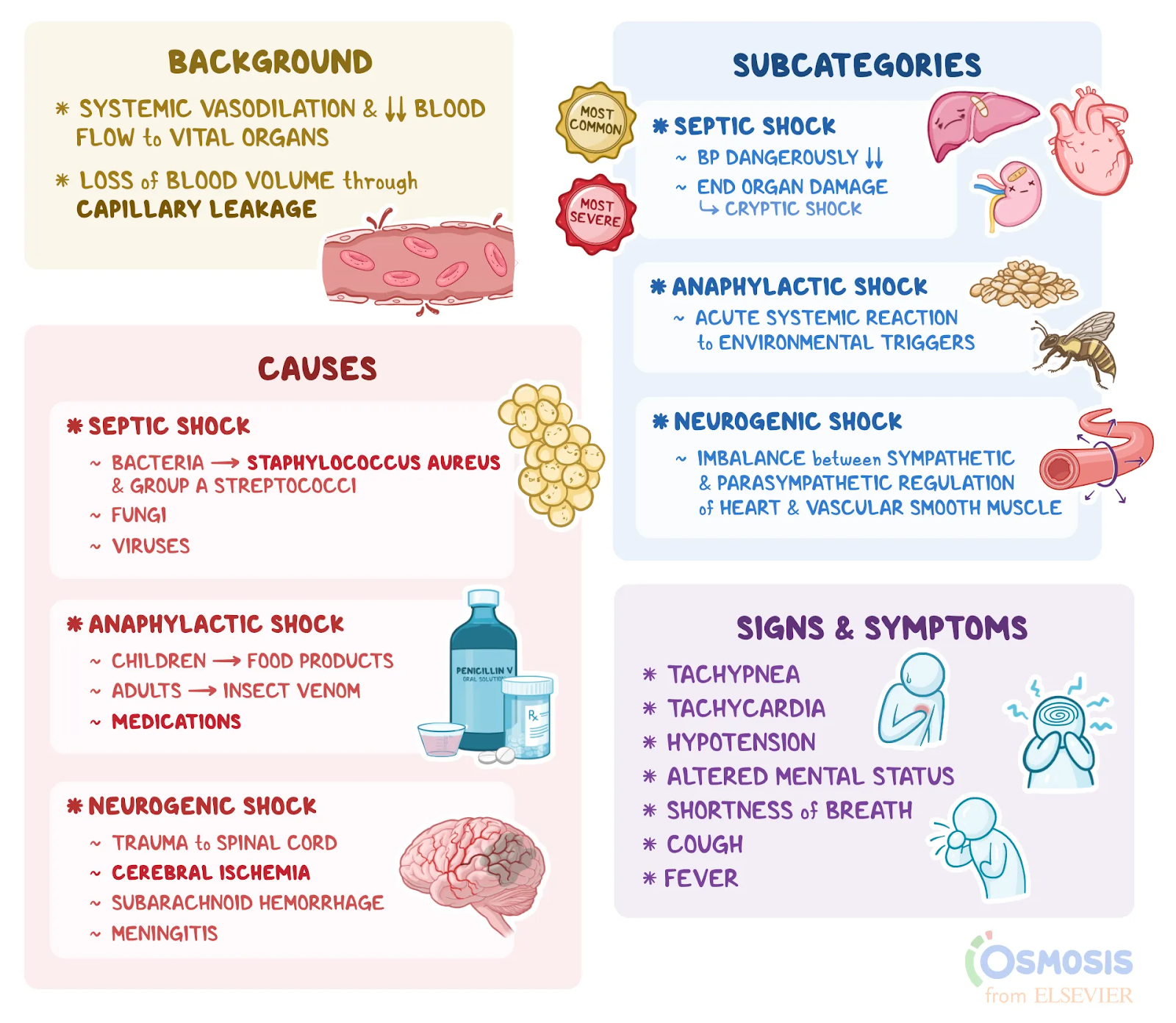
Three main types of distributive shock
- septic shock: the condition where an infection causes the individual's blood pressure to drop to a dangerously low level. half of the cases of septic shock, those with end-organ damage will present with cryptic shock, where blood pressure readings are normal but there is still inadequate tissue perfusion
- anaphylactic shock: an acute systemic reaction to environmental triggers, including allergic reactions to foods, such as nuts, or insect bites.occur at any age regardless of prior history and has proven to be fatal in 0.7 to 2 percent of cases. Mortality is exacerbated in those with asthma.
- neurogenic shock: state of imbalance between sympathetic and parasympathetic regulation of the heart and vascular smooth muscle. results in profound vasodilation, or capillary enlargement, with maintained blood volume but relative hypovolemia. Blood is then inadequately distributed in the body, leading to a loss of pressure and perfusion.
Distributive Shock: Septic
Septic shock occurs due to sepsis and this leads to major decreased tissue perfusion.
Sepsis is an invasion of microorganisms in the body. (bacteria, fungus, virus. or parasite)
When the bacteria invade capillary veins, the immune system acts as amplified. => Sepsis is the body’s amplified response to infection! (Think of septic shock being the end result of sepsis). 1 in 3 who die in a hospital have Sepsis (CDC.gov)
Causes ( pathophysiology): bacteria specifically Staphylococcus aureus and group A streptococci. a form of septic shock associated with vaginal tampon use, recent surgery, and open wounds. Lastly, fungi, such as candida, and viruses can also cause sepsis.
(Septic Shock risk Factors:Suppressed immune system, Extreme age=infant/ elderly, People who’ve receive an organ transplant, Surgical procedure=anything invasive, Indwelling devices=foley, central lines, trachs etc, Sickness=chronic DM, alcoholism, renal failure, liver failure)
Changes to V/S: CO low, low SVR ( major vasodilation)
persistent hypotension less than SBP 90
ㄴ even with large fluid replacement, need vasopressors(Norepinephrine)
to keep MAP > 65.
ㄴ > 2mmd/L lactate
(MAP: how well those vital organs are being perfused)
Other notable S/S:
early: “warm=compensation: hyperdynamic (vasodilation) warm/flushed skin, low BP, tachycardia, increased respiratory system, restless, anxiety
late: “cold=uncompensated: hypodynamic: vasoconstriction, cold/ clammy skin, severe hypotension, HR increased, RR increased, Oliguria, Coma, hypothermia, CO low
Treatment (Medication + Nursing Intervention)
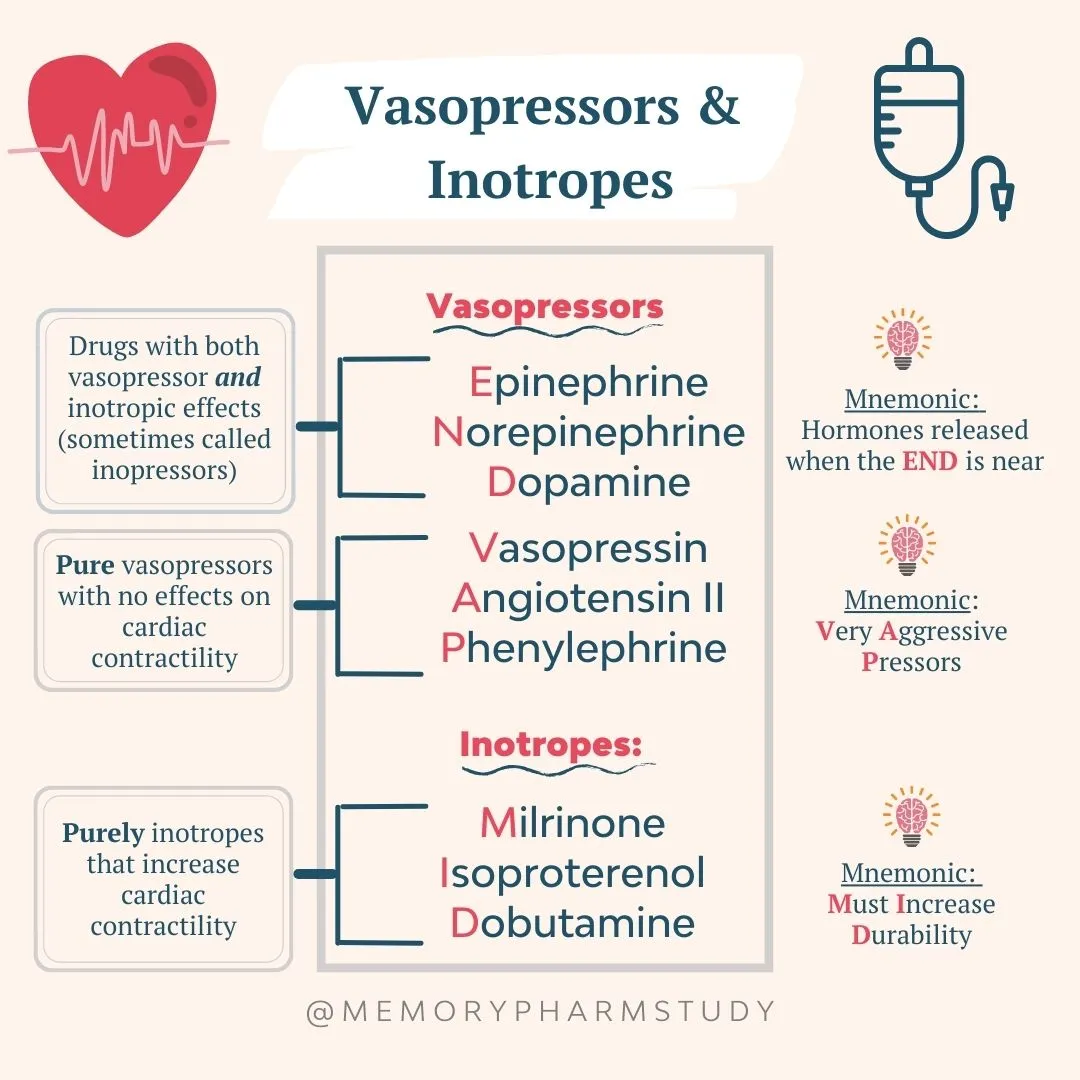
- increase perfusion: vasoconstriction, (epi or norepinephrine) before: fluid resuscitation
- oxygen therapy: To help you breathe more easily, you'll be given oxygen through a face mask
- Fight microorganism: blood cx then treat antibiotics => decrease inflammation
- nutrition
- control blood glucose level
====================================================================
“easy way to memorize: Septic Shock treatment”
ㄴ Start with antibiotics: administer within 1st hour… improves patient outcomes, cultures
needed before… however don’t delay antibiotic therapy
ㄴEnteral Nutrition: early: helps with GI integrity, Nutrition plays an important role within immune health, healing, and helps with stress ulcer prevention. GI drugs may be ordered (eg. famotidine) to help with ulcer prevention.
ㄴProtein Activated C: has anti-inflammatory & antithrombotic effects, eg, drotrecogin alfa most effective if started with 24`48 hours… watch for bleeding!
ㄴTitrate Vasopressors (MAP>65 mmHg): norepinephrine, used when fluid replacement is unsuccessful. cause vasoconstriction and increase SVR.
ㄴInotropes: eg: dobutamine, may be added if there is still low tissue perfusion, helps increase the strength of the heart’s contractions.
ㄴCrystalloids or Colloid Solutions: used as first initial treatment… if not working then vasopressors are added to treatment. successful if SBP >90 and CVP within normal range 8~12 mmHg. unsuccessful if persistent hypotension and CVP is less than 8mmHg
ㄴSteroids (corticosteroids…Low-dose): used in some patients to help decrease the amplified inflammation by the immune system, especially if the patient isn’t responding to vasopressors.
ㄴHemodynamic monitoring: will have a central venous/arterial catheter to help assess tissue perfusion and filling pressures in the heart. eg: CVP: filling pressure in right side of heart; PAWP: filling pressure in the left side of the heart.
ㄴOxygenate!: keep O2 Sat >95%,, tissues need oxygen!, at risk for ARDS… most patients need intubation with mechanical ventilation.
ㄴCultures!: collect before starting antibiotics, helps identify microorganisms causing the infection so appropriate antibiotics can be ordered.
ㄴKeep glucose <180mg/dL: prevent hyperglycemia.. this affects the immune system and healing. started on an insulin gtt to control.
monitor serum lactate levels: >2~4mmol/L abnormal…shows cells are struggling for oxygen and have switched to anaerobic metabolism.
monitor UOP(Foley insertion): >30ml/hr…if low, kidneys are failing due to decreased tissue perfusion.
===================================================================
Inotropic medicines (inotropes), such as dobutamine, stimulate your heart. They increase the strength of your heartbeat, which helps get oxygen-rich blood to your tissues and organs, where it's needed
Vasopressor: dopamine, adrenaline, noradrenaline
What is included in your nursing intervention/treatment for sepsis? Explain in terms of the 1-hour bundle and the 6-hour bundle.
1 hour:
- measure lactate level,
- collect two sets of blood culture( different sites)
- administer broad spectrum antibiotics within 1 hour
- initiate fluid bolus for hypotension or LA>4mmol/L (30ml/kg)
- assess and document vital signs
within 6 hour:
- re-measure lactate level
- check BP after flood resuscitation
- in the event of hypotension Mean Arterial Blood Pressure (MAP<65mmHG) or Lactate LA>4mmol/L, assist if the patient require insertion of CVC
- administer vasopressors to maintain MAP>65mmHG
- Assess and document V/S in timely manner
Why do we need to measure lactate levels in sepsis management?
- elevated lactate is an indicator of poor tissue perfusion whereas improvement in lactate level indicates improvement in tissue perfusion and responsiveness to resuscitation fluids.
Distributive Shock: Anaphylactic
allergic reaction that can be deadly if you don’t treat it right away
Introduction of an allergen in the body that leads that leads mast or basophils cells to release histamine.
Histamin: decreased tissue perfusion =>shock, VAsodilation=low BP, HR elevated, increased capillary, itching, swelling, low CO. Bronchoconstriction= respiratory failure, contraction of GI = Nausea, vomiting,
Causes: an allergy to food (shellfish,peanuts, eggs,milk), insect bites, latex, physical exercise, unknow(Idiopathic), certain medications (contrast dye, vaccines, NSAIDS, Antibiotics[PCN=penicillin])
Changes to v/s: low BP, HR increased, dyspnea
other notable S/S:
- Anaphylactic reaction: (immunological) IgE related, needs sensitization for reaction to occur
- Anaphylactoid Reaction: (non-immunological) not related to IgE, no sensitization required, can happen 1st exposure,
- IV contrast, NSAIDS, Chemical agents.
Respiratory: dyspnea, wheezing, swelling upper airways “tightness” and speak, coughing, weary eyes, stuffy nose
Cardiac: hypotension, SBP < 90, increased HR, (lose consciousness)
GI: vomiting, nausea, diarrhea, pain
Skin: itchy, red, swollen (vasodilation)
Treatment ( medications + nursing interventions):
- Prevention! (Assess[allergy, anaphylactic shock], document[see doctor’s history], Avoid)
- recognize signs and symptoms and act fast!
ㄴAllergen (remove it)&Airway (high-flow oxygen)
ㄴCall Rapid response (start CPR, if needed, until help arrives)
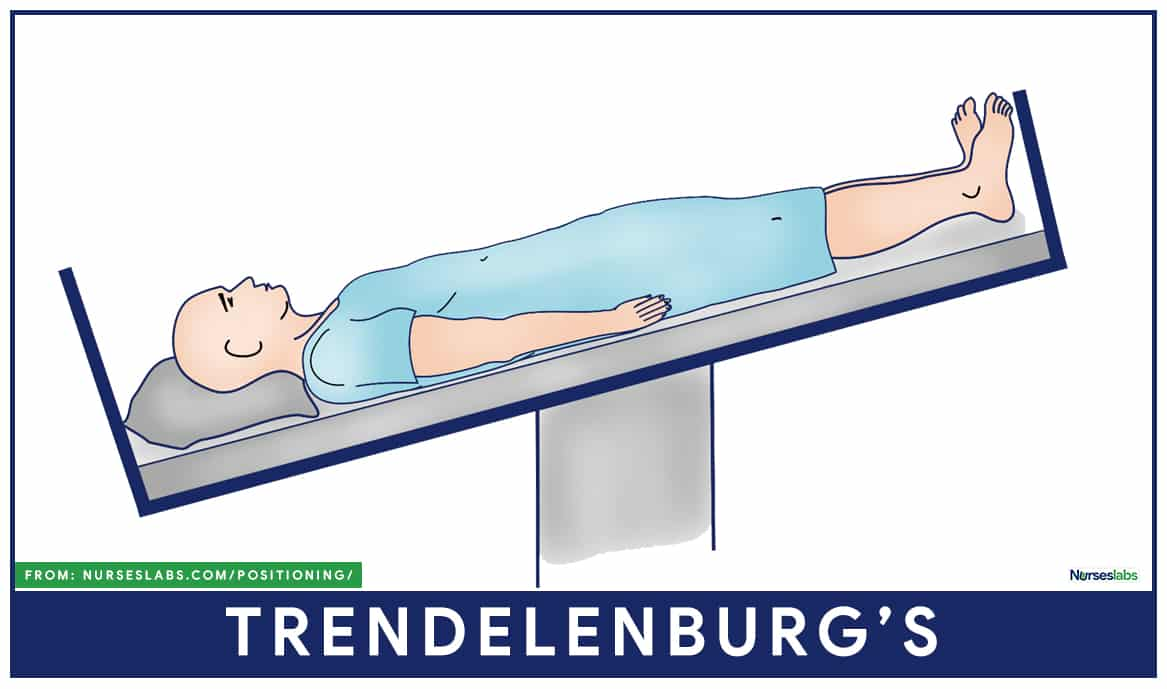
ㄴTrendelenburg position: increase venous return to the heart, which will help increase cardiac output and blood pressure)
ㄴFirst-line drug is Epinephrine (vasoconstriction, bronchodilation)
ㄴAdminister per MD order ( IV fluids, albuterol(nebulizer: dilate airway),antihistamines (Diphenhydramine:H1, Ranitidine: H2), Corticosteroids
ㄴStay and monitor patient ( biphasic anaphylactic: occur again.
ㄴTeach! (Avoid allergen, wear a medical alert bracelet: carry Epipen always, replace it when it expires, know how to prepare and administer, massage injection site for 10 secs, call 119 immediately!)
Distributive Shock: Neurogenic
Neurogenic shock occurs when the sympathetic nervous system loses their ability to stimulate nerve impulses. (they used to regulate diameter of vessels, but in this condition they lose its ability)
ㄴ this leads to hemodynamic changes such as vasodilation (decrease SVR, afterload V), hypotension, venous blood pooling (preload V), CO decreased. Bradicardia
sympathetic nervous system (SNS) aroused from Autonomic nervous system.
Autonomic Nervous System Controls that we can’t consciously control like : HR, BP, Digestion, Respiratory rate, Urination, pupillary response and more.
Autonomic Nervous System divided in two:
- parasympathetic : “rest and digest system”
- Sympathetic: “fight or flight” (keeps you alive, see the danger, increase, HR, BP,
ㄴ role in controlling vasomotor tone, which regulates diameter of vessels.
-high rate of firing- vasoconstriction, epinephrine, norepinephrine
-low rate of firing- vasodilation
Causes: spinal cord injury ( above T6), autonomic nervous system toxins, Guillain-Barre syndrome, spinal anesthesia, transverse myelitis.
Other notable S/S: hypotension, bradyarrhythmia, flushed, warm skin that gets cold and clammy later, lips and fingernails that look blue, lack of full consciousness
Treatment & Nursing Intervention:
protected the spine!
- keep spine immobilized: ex) cervical collar, log-rolling patent, using a backboard etc.
assess and manage the airway!
- may need intubation and mechanical ventilation, if respiratory failure is present!
maintain Tissue perfusion!
- goal: MAP to be 85~90mmHg to maintain perfusion to organs (especially spine)
- how?: IV fluids,,, crystalloids (used with caution) watch for Fluid volume overload, suspect FVO if patient has dyspnea, crackles, edema, high CVP/PAWP etc
- fluid not working?
ㄴ use vasopressors (causes vaso constriction) increase SVR, BP, CO
ㄴ use positive inotropes: Dopamine (vasoconstriction and increase HR)
- Bradicardia? Atropine (increase HR) blocks the parasympathetic effects on the heart which is causing the slow HR,,,-> may need temporary pacing
- warming devices for hypothermia (check body temperature=BT)
- foley placement: some patients lose bladder function. urinary output 30ml/hr
- prevent of DVT(deep vein thrombosis)
ㄴROM daily, compression stockings, anticoagulants(avoid crossing legs or placing pillow under knees…compromises circulation)
Hypovolemic Shock: low blood volume
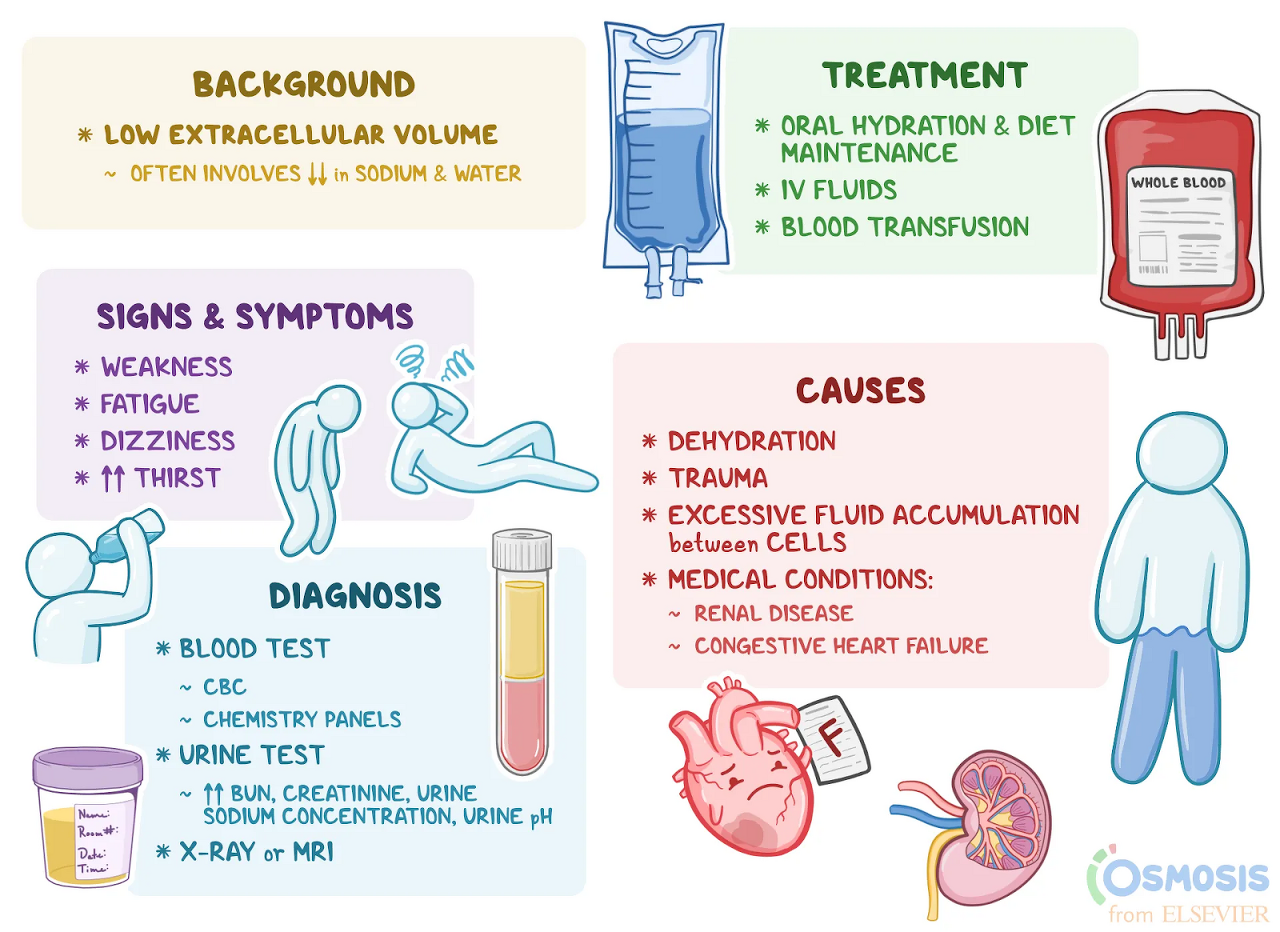
occur when low fluid volume in the blood (intravascular system)
intravascular space: space that contains the volume of blood in a person’s circulatory system.
when there is low blood volume, low CO, if the person loses 15% or more blood volume, they undergo signs and symptoms of shock.
Causes:
Relative Hypovolemic Shock: INSIDE fluid shift from the intravascular system. fluids or blood collecting or leaking inside the body
- internal bleeding,
- third-spacing of fluid…severe burns due to increased capillary permeability,
- long bone fractures,
- damage to organs like the pancreas,
- massive vasodilation …sepsis.
Absolute Hypovolemic shock: OUTSIDE fluid shift from the intravascular system. fluid leaves the body!
- massive bleeding from surgery or injury
- excessive fluid loss: vomiting, urination, diarrhea, swearing…many times caused by a disease process or endocrine disorder.
Changes to v/s: low BP, tachycardia, increased RR
preload: amount ventricles stretch at the end of diastole (end-diastolic volume)
stroke volume: amount of blood the left ventricle pumps each beat (50~100ml)
4 types of stages of Fluid volume loss
- Class I: <15 %(750ml) -> body compensates to maintain CO, asymptomatic
- Class II: <15~30%(750~1500ml) -> low CO = SNS, RAS, shunting to blood (vasoconstriction, => blood volume increased, aldosterone, ADH, preload increased)
- Class III: <30~40% (1500~2000ml) ->compensation not working, low CO, malfunctioning organs. confusion, agitation, skin cool, clumsy
- Class IV: <40~50% (>2000ml) -> death near. significant abnormal , oliguria, tachycardia, hypotensive.
Other notable S/S: confusion, oliguria, skin color change, etc.
Treatment ( medications + nursing interventions):
Fluids (Crystalloids):
ㄴNormal saline or Lactated Ringer’s: they add more fluid to the intravascular system… This increases preload, stroke volume and cardiac output!
ㄴWatch for: fluid volume overload… hemodynamic monitoring: elevated CVP or PCWP(pulmonary capillary wedge pressure: left side pressure), fluid in the lungs… cracked.
- These solutions are able to diffuse through the capillary wall so less fluid remains in the intravascular space.
ㄴ Noraml Saline or Lactated Ringer’s Most commonly used!, 3:1 rule
- 3:1 rule: for every 1ml of approximate blood loss, 3 ml of crystalloid solution is given: 750ml loss = 2,250 ml
Fluids (Colloids):
ㄴconsists of large molecules that cannot diffuse through the capillary wall so more fluid stays in the intravascular space for longer (more expensive, patients can have an anaphylactic reaction, monitor for fluid overload.)
eg: albumin, hetastarch
if the patients need a large amount of fluids needed, then warm them to prevent hypothermia. Hypothermia can alter clotting enzymes, keep the patient warm, but not to the point of sweating.
Blood & Blood products (PRBC, Platelets or Fresh Frozen Plasma (FFP))
- PRBCS: help replace fluid and provides the patient with hemoglobin, which will carry oxygen to deprived cells (crystalloids and colloids can’t do this)
- may be used when the patient is not responding to crystalloid fluid challenge, experienced severe bleeding/severe hypovolemic shock etc.
- Platelets: uncontrolled bleeding to help with thrombocytopenia
- FFP: if patient needs clotting factors * monitor for transfusion reaction with these products**
Nursing: oxygenation & circulation, mech-ventilator, bleeding? adeq. perfusion?
I/O, Foley (monitor urinary output), IV-access stat ( 2 sites, large-cannula, more than 18G), central line & hemodynamic.
modified Trendelenburg position=> increased venous return,
labs: Hgb, Hct, ABG, electrolytes, CBC (BUN, creatinine levels for kidney function), lactate level.
Cardiogenic Shock
The heart can not pump enough blood to meet the perfusion needs of the body.
ㄴ filling/ contraction issue or dysrhythmia, structure defect.
ㄴ not due to loss of blood volume to pump.
ㄴ low CO => low perfusion => decreased O2 supply to cells that make up organs and tissues
Cardiac Output: amount of blood pumped by the heart per min. (4~8L/min)/ HR+SV
Stroke Volume: amount blood pumped by ventricle each beat (50~100ml)
stroke volume influenced by 3 factors:
- preload: amount the ventricle stretches at the end of diastole: end-diastolic volume
- afterload: pressure the ventricle must pump against to squeeze blood out of the heart
- Contractility: how well the muscle cells contractL strength of the heart within contractions
Cardiac Index= CO / body surface area
Causes: Acute MI (especially left ventricle, contraction issue), pericardial tamponade(too much fluid around the heart can’t fill), dysrhythmias, myo-endo/carditis, valves, septum
Changes to v/s: RR increase, SBP <90, HR increased.
Other notable S/S:
Heart: weak, not-pumping blood efficiently
backflow of blood: => lungs => pulmonary edema, decreased Ox, RR increased. HR
increased, PCWP& PAWP increased>18mmHg
ㄴRight side: JVD, high CVP
PCWP/PAWP: normal range (4~12mmHg)
Low CO:
- weak peripheral pulses
- SBP < 90mmHg
- Chest pain
- Cardiac index < 2.2 l/min/m2
Brain: CPP decreased - cells can’t perfused, mental changed (confusion, agitation)
Kidney: perfusion decreased and activate RAS => keep sodium H2o => Oliguria < 30ml/hr,
BUN Creatinine increased.
Skin: cool, clammy, capillary refill delayed greater than 2 seconds.
Treatment (medications + nursing interventions):
- medical Tx goals: perfusion, CO, ventilate-mech, diuretics
- maintain hemodynamic: monitoring mech-ventilation (respiratory failure)
- central line placement (measure CO)
- monitor symptoms and signs of adequate tissue perfusion (BP, skin color, Cap-refill, UOP(BUN/Creatinine), mental status, lung sounds (crackle), rhythm.
- Lab: Cardiac markers (elevated Troponin: released when there is injury to the heart muscle’s cells, BNP: released by the ventricle’s heart cells due to stretching from high blood volume in the ventricle)
- Chest x-ray: pulmonary edema
- Serum lactate > 4mmol/L: cells switch from aerobic to anaerobic metabolism… lactic acid accumulation is the result of this switch, Acidosis: decrease in Blood PH <735
- medication:
diruetics (furosemide IV: watch K+ 3,5~5mEg/L: decrease workload of heart (hypotension & F/E)
Vasopressors: constriction of vessels (Norepinephrine), positive inotropic effects (Dobutamine: side effects are worsening hypotension like vasodilation, in this case change the drug to dopamine or epinephrine)
IV fluid used with extreme caution because of pulmonary edema
Intra-aortic balloon pump: device placed to help improve coronary artery blood flow to increase CO. => deflated during systole => inflated during diastole
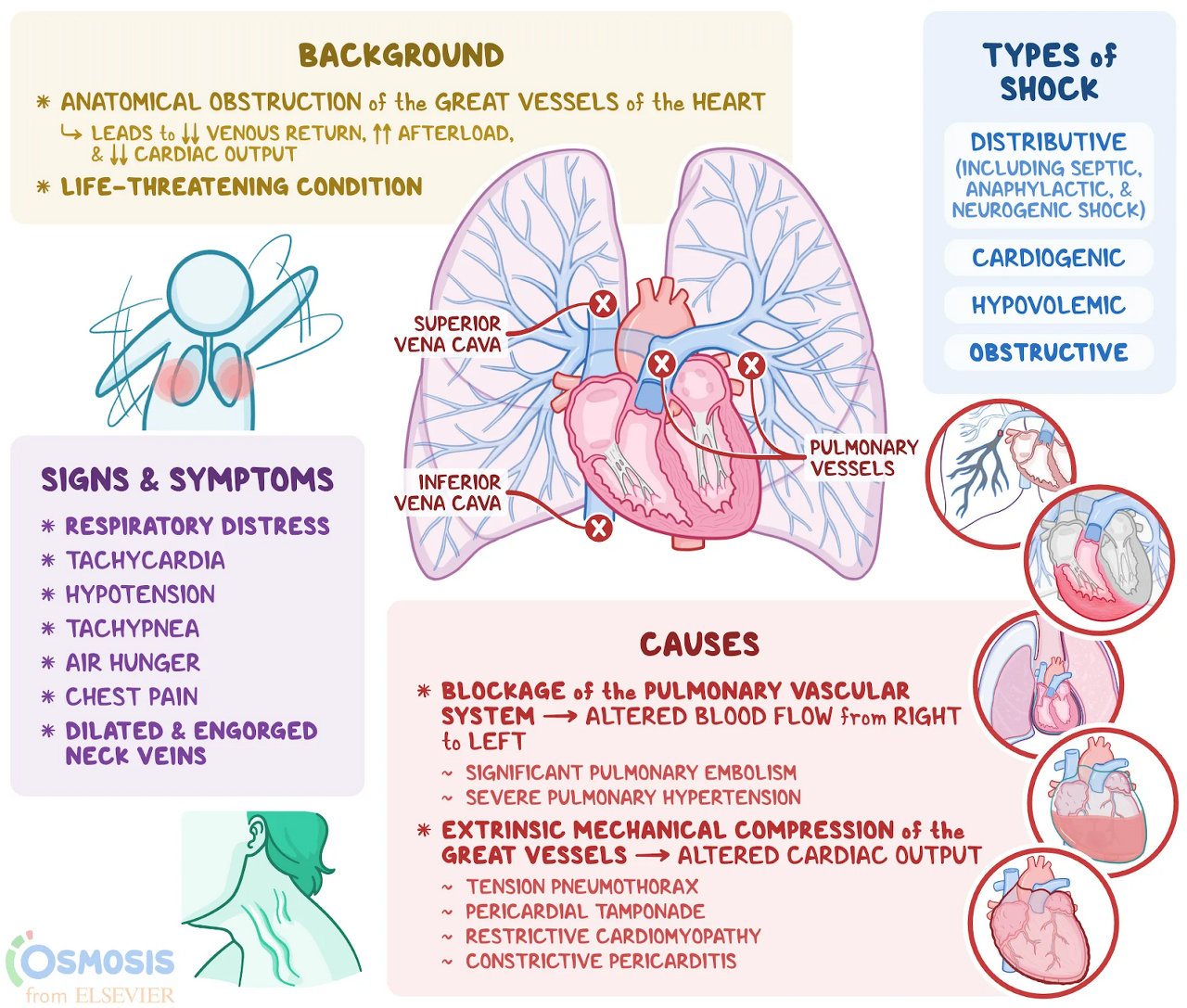
Obstructive Shock
Obstruction of the superior vena cava, inferior vena cava, and pulmonary vessels that leads to decreased venous return, resulting in decreased cardiac output.
Causes:
- tension pneumothorax: air in the pleural cavity => constriction of the heart
Treatment: x-ray to find out deviated location of the thorax. => chest tube
pleural cavity: space that surrounds lungs.
- cardiac tamponade: excessive fluid in the pericardial sac in the heart=> increased pressure of the heart that lead decreased venous return and the ventricle's size shrinked.
Becks Triad: muffled Heart sounds, JVD (jugular venous distension), Hypotension(narrow pulse pressure:systolic=diastolic)
treatment: durian the fluid (CT, pericardiocentesis, pericardial drain)
- Constrictive pericarditis: infection
Treatment: anti-inflammatory, steroids, pericardectory
- Aortic stenosis: mur mur echo sound
Treatment: valvuloplasty, New valve, open heart surgery: repair valve
- Pulmonary Embolism: most common causes that can lead DVT
Treatment: dissolve by TPA, TNK, heparin, remove embolus by surgery
Changes to v/s: RR increased, HR increased, Low BP
other notable S/S: pallor’s cyanosis
Treatment ( medications + nursing interventions):
- Lab: serum lactate
- ABG
- obstruction?=> relieve obstruction by Chest tube, drainage for effusions and heparin dosages.
What is the difference between cardiogenic shock and obstructive shock?
Cardiogenic shock, the heart can’t pump the right amount of blood that the body needs. This occurs most commonly after a heart attack stuns or permanently injures a large portion of your heart muscle, resulting in poor output.
Obstructive shock, there are some obstructions in the blood so, the body can’t get enough blood that they need. A large blood clot in your pulmonary artery.
======================================================================
What is Sepsis and Septic Shock?
- Sepsis is defined as a life-threatening organ dysfunction due to a dysregulated host response to infection
- Septic shock is a subset of sepsis where particularly profound circulatory, cellular and metabolic abnormalities substantially increase mortality.
'간호사 공부 모음' 카테고리의 다른 글
| IICP (Increased Intracranial Pressure) (0) | 2023.07.02 |
|---|---|
| 뇌혈관 질환: 간단한 병태생리 (0) | 2023.07.02 |
| Central lines + CLABSI Bundle (0) | 2023.07.01 |
| 신경계 사정: Neurological Assessment (0) | 2023.07.01 |
| 3년차 간호사 시점... (0) | 2023.03.09 |



