CRRT ( Continuous Renal Replacement Therapy)
Describe the functions of the kidneys using the mnemonic: A WET BED:
A: acid/base balance
W: water balance regulation
E: erythropoiesis
T: toxin removal
B: blood pressure regulation
E: electrolyte balance
D: vitamin D activation
Do you have experience with CRRT? What is CRRT?
CRRT stands for continuous renal replacement therapy and it is a non-stop, 24 hour dialysis. It helps patients with acute kidney injury (AKI) and fluid overload.
What are your nursing responsibilities for patients on CRRT? (Mention about special labs such as electrolytes and ABGs, physical assessment, and hemodynamic monitoring, etc?
- hyperkalemia
- hyponatremia
- hypothermia
- hypotension
- metabolic acidosis
What CRRT alarms have you dealt with and how did you troubleshoot for each alarm?
LOW ARTERIAL PRESSURE ALARM
- kinked or clamped line -> remove kink/ clamp
- clotted line -> declot access
- access device against vessel wall -> consider switching limbs
- hypovolemia -> stop UF, decrease blood flow rate
HIGH VENOUS PRESSURE ALARM
- kinked or clamped line -> remove kink/ clamp
- clotted line -> declot access
- positional vascular access obstruction -> switching consider limbs
DISCONNECTION ALARM
- line separation or disconnection from patient (rare) -> check circuit and patient and if no disconnection then override alarm
- circuit kinked or clamped before pressure sensor -> declamp line
- clot excluding pressure sensor -> evaluate for circuit change
- blood pump speed too slow relative to catheter performance -> increase set blood flow rate
AIR IN THE CIRCUIT ALARM
- presence of small air bubbles in circuit (often due to bicarbonate CO2 coming from hemofiltration bags) -> follow instructions for degassing
- line disconnection at arterial access -> stop session
- turbulence close to sensor -> override alarm
FLUID BALANCE ERROR
- effluent or hemodialysis/ filtration bags moving or incorrectly hanged -> wait for bags to stabilise, stop or reposition them on scales
- kinking in effluent or hemofiltration/ dialysis bags -> remove line kinking
- machine occassional error -> override
- machine systemic error (if more than 10 times without reason in 3 hours) -> change machine and do not reuse before technical assistance
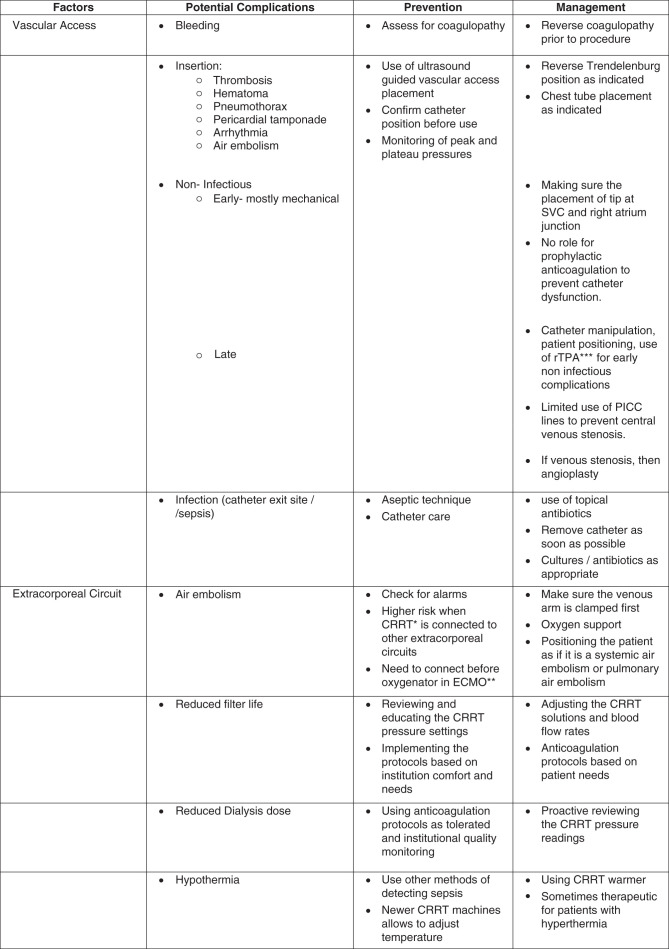
What are some complications that are associated with CRRT? How will you prevent these complications?

ECMO: extracorporeal membrane oxygenation
Have you worked with patients on ECMO? Tell me what is ECMO,
ECMO (extracorporeal membrane oxygenation) is a type of artificial life support that can help a person whose lungs and heart aren’t functioning correctly. ECMO continuously pumps blood out of your body and then sends it through devices that add oxygen and remove carbon dioxide. It then pumps the blood back into your body.
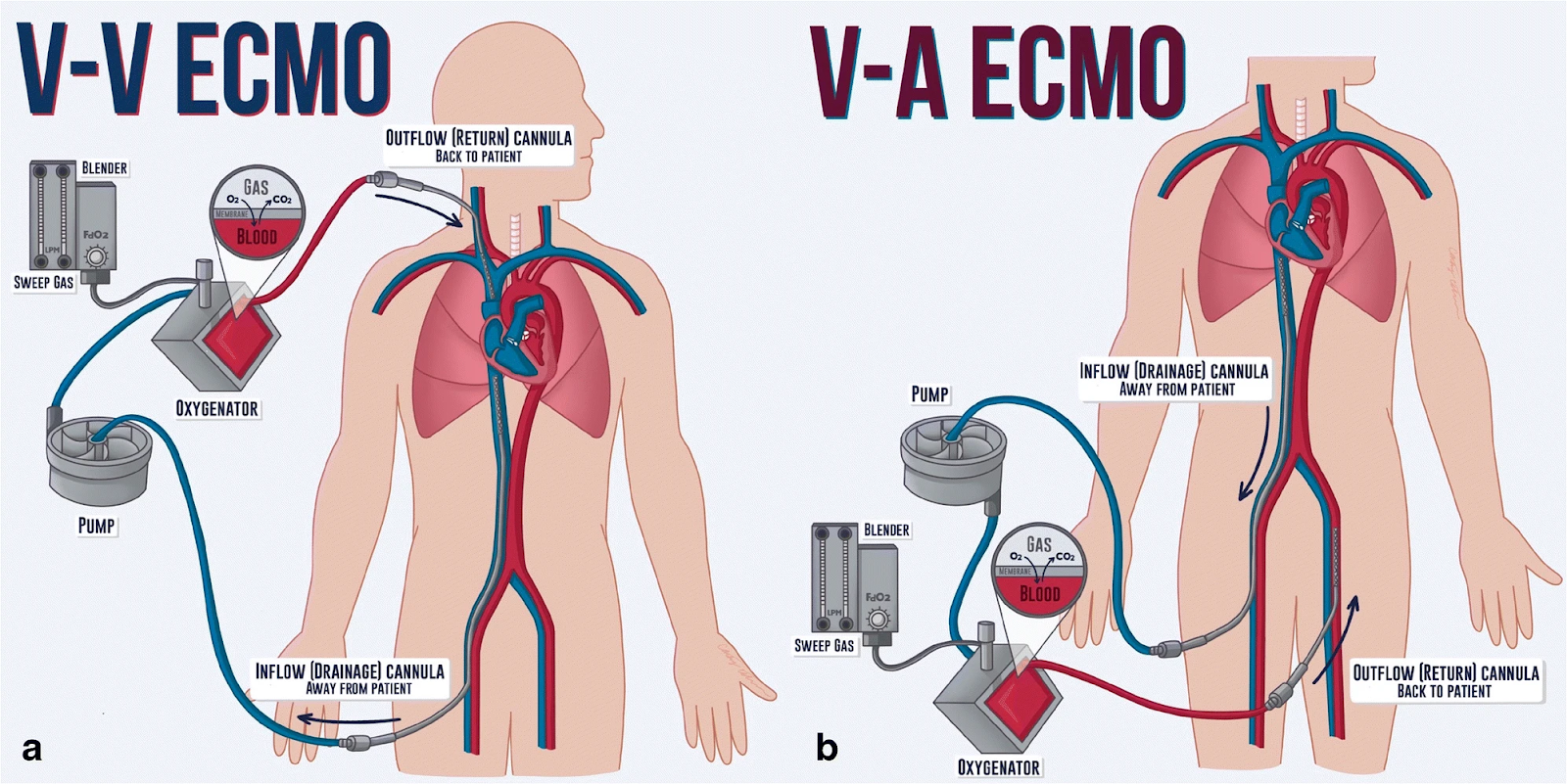
Describe the 2 different modes of ECMO (VA&VV) and explain the indications for each mode. VV: veno-venous/ VA: veno-arterial
VV ECMO drains blood from the venous system, reinfuses blood into the venous system, and provides gas exchange but no direct cardiac support. In contrast, VA ECMO drains blood from the venous system, reinfuses into the arterial system, and provides complete cardiopulmonary support
What are some complications associated with ECMO?
- Bleeding.
- Blood clot (thromboembolism)
- Blood clotting disorder (coagulopathy)
- Infection.
- Loss of blood in hands, feet or legs (limb ischemia)
- Seizures.
- Stroke (part of the brain is damaged by loss of blood or by a blood vessel that bursts)
Explain your nursing responsibilities for patients on ECMO? ( How will you prevent the complications)?
- Chest Tubes
How familiar are you with chest tubes? What types or brands of chest tubes have you used?
What are the indications of chest tubes?
- pneumothorax
- hemothorax
- pneumomediastinum
- pleural effusion
- post-operative drainage
- emphysema
- chylothorax
- prophylactically in high risk patients needing mechanical ventilation (stiff lungs)
What are the 3 chambers in the chest tube (Atrium)? Explain the functions or purposes of each of the 3 chambers
- fluid collection chamber
- Receive drainage form the patient
- chamber may be single or divided into a major and minor chambers
- The chambers are calibrated in 2 ml increments up to the 200ml point, and in 5 ml increments over this point.
- amount of the drainage can be calibrated
- Water-seal Chamber
- the water-seal chamber should be filled to the 2cm mark with sterile water ( do not fill above 2 cm line)
- When this chamber is filled with fluid to the 2 cm line, a 2 cm H2o seal is established, which keeps air from entering the pleural cavity, allowing air to pass down the narrow channel in the chamber, to bubble out at the bottom of the water seal.
Has three purposes:
- it acts as a one-way valve to allow air to escape from the pleural space
- it measures the amount of negativity in the patient’s chest cavity
- it allows for observation of the degree of air leak
As intrapleural pressure changes (e.g. with breathing), the water level will swing up and down. this is known as “TIDALING”
An air leak is present when air bubbles can be seen going from right to left in the air leak monitor at the base of the water seal chamber
- continuous bubbling: there is a persistent air leak
- intermittent bubbling: indicates an intermittent air leak
- no bubbling: means that there is no air leak
“Stripping” or “milking” the drainage tubing can cause extremely high levels of negativity. use the high negativity relief valve to restore negativity to prescribed levels.
- Suction Chamber
- the chamber is filled to the ordered level (usually 20 cm)
- it means it generates -20 cm H2O
- the level of suction imposed is determined by the fluid level (not the suction regulator)
- Increasing suction at the regulator will not increase suction pressure in the pleural cavity: it will just increase the rate of air flow through the system.
- by adding or removing water in the suction control chamber, the amount of suction imposed on the patient can be controlled.
ㄴ the lower the water level, the lower the degree of suction
ㄴ the higher the level, the higher the suction level will be.
- Use of suction helps overcome an air leak by improving the rate of air and fluid flow from the patient.
- suction should be regulated to produce gentle bubbling within the chamber.
- suction may be discontinued to transport the patient, or it may be discontinued 4 hours before chest tube removal.
Describe the steps on how to set up the disposable underwater-seal drainage system.
step 1: the water seal chamber should be filled to the 2cm mark with sterile water, using the syringe provided with the pack. the water should turn blue once the water seal is filled. This will allow air to pass down the narrow channel in the chamber, to bubble out at the bottom of the water seal.
step 2: connect the suction control chamber with desired suction pressure level (-20cmH2O)/ remove the tethered vent-plug, pour in the sterile water, and replace the vent-plug.
step3: insert the steeped connector into the patient’s chest tube. chest drain should be connected to the patient prior to initiating suction.
step 4: applying suction:
What does tidaling and bubbling (intermittent or rapid) indicate?
- as intrapleural pressure changes (e.g. with breathing), the water level will swing up and down, and this is known as tidaling
- bubbling: air leak presents.
What are some complications associated with chest tubes?
- pain
- pneumothorax
- bleeding
- skin necrosis at suture site
- infection at insertion site
What is your nursing role post-removal of chest tubes?
- ensure that your patient receives adequate analgesia
- pain assessment & management
- document baseline status - assess for presence of cyanosis, vital signs, spO2, bilateral lung auscultation, respiratory rate and effort, and LOC, as per unit protocol
- check all tubing connections to ensure they are airtight- secure with adhesive tape as per unit protocol, ensuring that the tube is not being pulled.
- keep the tubing and drainage system positioned below the patient's chest at all times.
- reinforce patient and family education as needed.
- observe for possible complications
'간호사 공부 모음' 카테고리의 다른 글
| Ileus (0) | 2023.08.18 |
|---|---|
| ETT Intubation (0) | 2023.07.06 |
| 사우디 간호사 면접 준비 _1탄 (0) | 2023.07.06 |
| Stroke Code (0) | 2023.07.05 |
| PCA Stroke: 후두엽 (Visual Cortex) (0) | 2023.07.05 |



